Two medications that have been in most homes for decades, if not over a century, are Aspirin and Tylenol. These antipyretics/analgesics are mainstays in my collection, and it would remiss of me not to feature items from the collection together, as well as explain why their use was so widespread then, and remains so today. Another popular pain medication, Phenacetin, is also present in the collection, but is not widely known anymore. Remember always that just because it is a medication does not mean it has been studied long term, or is safe. As one of my college professors stated, “At some point, the longer you are on something, the more you become part of the experiment.”
Aspirin
Tylenol
Phenacetin
Acetylsalicylic Acid
Aspirin, also known as acetylsalicylic acid, is a popular fever reducer, pain reliever and anti-inflammatory that has been used for over 2400 years. It is commonly used to reduce mortality due to cardiovascular disease when used as low dose (81 mg, formerly known as “baby aspirin”). Its precursor is found in willow leaves. In 1853, a French chemist, Charles Gerhardt, created acetylsalicyclic acid by treating sodium salicylate with actyl chloride. In 1897, the German pharmaceutical company Bayer noticed it worked as well as other salicylates but with less irritation. By 1899, Bayer was using the word “Aspirin” in place of its chemical name, and which it is more widely known as today.
Charles Gerhardt, chemist
Acetylsalicylic acid is an irreversible COX-inhbitor, which prevents arachidonic acid from transforming into protoglandins and prostanoids, which are involved with the pain cascade, and inflammation/vasoconstriction effects, respectively.
The main side effect to be concerned about is its effect on the gastrointestinal tract, which can result in bleeding (ulcers). Its use should also be avoided in children under 14 who have had a fever/recent illness. There is a rare illness called Reyes Syndrome, in which 90% of the cases occur after viral infection recovery in pediatrics when aspirin is taken. This is a syndrome of 5 stages, which start with rash and vomiting, then escalates to a symptomatic fatty liver, coma/cerebral edema, continued elevated liver dysfunction, and finally, seizure/death. In 1986, the FDA mandated labeling on as aspirin products warning against use in children, with the exception of Kawasaki’s Disease (which is an inflammation of mucotaneous lymph nodes and prolonged fever).
St. Joseph Aspirin advertisement for Asian Flu, 1958 (“the best aspirin for your child”)
St. Joseph Aspirin for children, 1964 advertisement
Hicks Capudine, which contains a salicylate with caffeine, due to its synergistic relationship
As with many other NSAIDs (non-steroidal anti inflammatory), when combined with caffeine, the result is a synergistic compound that is more effective than the NSAID alone. In fact, aspirin combined with both caffeine and acetaminophen is a first line treatment for migraines.
Acetaminophen
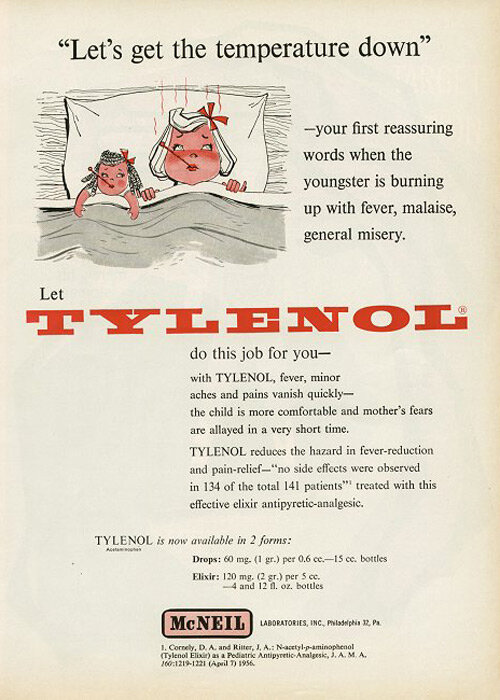
Tylenol advertisement, 1958
Tylenol, also known as acetaminophen (APAP), is a popular fever reducer and pain reliever. It, like aspirin, decreases COX in the body, but is not a direct inhibitor. It works in the central nervous system and therefore has NO anti-inflammatory effects. It was first created in 1877.
It is better tolerated than aspirin due to decreased bleeding risk.
One of the main concerns with Tylenol is liver toxicity. Tylenol is metabolized into a liver hostile compound, which is normally cleared by glutathione (made by your body). If there is too much Tylenol, this toxic product can build up and damage the liver. Alcohol also has a toxic byproduct that requires glutathione to clear it, or it can also damage the liver.
In 2011, the FDA launched a public education campaign to increase awareness of its use. Many people did not realize acetaminophen, APAP , Tyenol and Paracetamol were all the same chemical, and that doses over 1000 mg, and over 4000 mg/day, could result in decreased hepatic function. The dosage for prescription combination products decreased, with many oxycodone combination medications changing from 600 or 500 mg to 325 mg. Tylenol also has a synergistic relationship for pain relief, but with opioids.
Endocet label, before dosage of APAP was limited by the FDA in 2011 (synergistic effect of oxycodone boosted by APAP)
Acetophenetidin
Acetophenetidin, or Phenacetin, is an analgesic and antipyretic synthesized by American scientist Harmon Morse in 1878, who also worked with osmosis (and is known for the Morse equation). In 1887, Bayer began manufacturing it for use as one of the first synthetic analgesics. It is a precursor to acetaminophen (whose synthesis is also credited to Mr Morse). In 1983, it was pulled from the market by the FDA due to its carcinogenic risk, increased evidence of kidney damage, and increased risk of cardiovascular associated deaths. In fact, famed aviator Howard Hughes is thought to have died of kidney complications due to regular use of phenacetin products.
Anacin advertisment (contains acetophenetidin)
Indian Anacin Advertisement (contains acetophenetidin)
Romind advertisement (contains acetophenetidin)